Our takeaways:
- COVID-19 may have a say in your ovulation timing.
- Ovulation tests can’t guarantee a pregnancy, but they can help you predict what your fertile days are with higher confidence given the uncertainties presented by the bigger environment.
- Different manufacturers of LH tests have very different recommendations on the best time of the day to test.
COVID-19 may have a say in your ovulation timing
Like many TTC (Trying to Conceive) couples, you have been trying to get a lot of things “right” when making a baby: a healthy diet, an active lifestyle, taking prenatal vitamins, getting solid 8-hour sleeps, and tracking your menstrual cycles, etc. However, there’s one important factor for baby-making that might not have even come across your mind: COVID-19.
(Now you may pause for as long as you need. I was as shocked too the first time I learned about this.) Yes, you read it right. COVID-19 can affect your chances of getting pregnant. But how? To what extent? Should I be worried? Here’s a quick summary for you based on what we know from reliable sources:
1. Some people may experience temporary changes in menstrual volume and menstrual cycle length due to COVID-19.
According to a study published in PubMed Central (A highly respected database from the National Institutes of Health), 25% of the 177 patients analyzed presented with menstrual volume changes, and 28% had menstrual cycle changes, mainly a decreased volume (20%) and a prolonged cycle (19%).
2. Levels of sex hormones didn’t differ significantly between those with COVID-19 and those without COVID-19.
The same study also analyzed the sex hormone changes in 91 patients during the disease. The data showed no statistically significant differences in all of the sex hormone concentrations between the COVID-19 patients and the controls. Subgroup analysis based on menstrual changes also indicated that there were no significant changes in sex hormone concentrations in either menstrual volume changes, simple cycle changes, or simultaneous volume and cycle changes.
3. Most people returned to their normal menstrual patterns 1 to 2 months after having COVID-19.
The good news from this study was that 84% returned to a normal menstrual volume, and 99% of patients returned to their normal cycle within 1–2 months after having COVID-19.
In addition to Covid infections, it’s worth knowing that other factors such as COVID-19 vaccines or pandemic stress can potentially play a role in the menstrual cycle changes. While the exact reason why COVID-19 may temporarily affect your period requires further study, what we know is that the old way of counting days based on your menstrual cycle to figure out the best baby-making/ovulation timing is probably less reliable now than ever.
Ovulation and Ovulation Tests
It’s been 2 consecutive months when my period lasted for 7+ days (vs 4-5 days in all my previous cycles). I didn’t suspect anything until I read the aforementioned study that reminded me of being COVID positive two months ago. There’s no way for me to prove if I belong to that nearly one-fifth of people with prolonged periods nor did I have confidence in my cycle returning to normal after 2 months like the rest of the 99%. So I decided to rely on ovulation predictor tests (OPK) to get my baby-making timing right.
As a refresher, ovulation is the process in which a mature egg is released from the ovary. After it’s released, the egg moves down the fallopian tube and stays there for 12 to 24 hours, where it can be fertilized.
1. How does the ovulation test work?
When your body gets ready to ovulate, it produces more luteinizing hormone (LH). The ovulation tests are designed to detect levels of LH in your urine. A positive result tells you that it’s time for you and your partner to have unprotected intercourse within 24-48 hours.
2. When to begin testing?
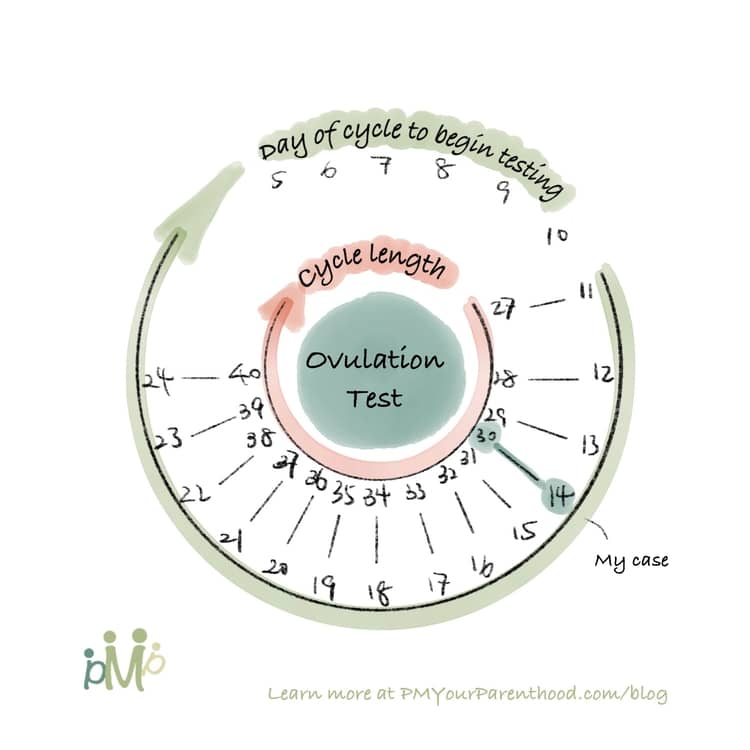
If you have regular cycles, you can refer to the diagram below to determine when to start testing. If you have irregular cycles or don’t know your cycle length (the duration from your first period starting day to the day before the next period starting day), you may begin testing 11 to 12 days after your first period day.
3. What time of the day should I be testing?
American College of Obstetricians and Gynecologists (ACOG) and the American Society for Reproductive Medicine (ASRM) do not have recommendations on when during the day to test, which may be part of the reason why different manufacturers of LH tests have very different recommendations (i.e: first thing in the morning vs after 12 pm). Make sure you read the instructions for your LH test. Here are some big brands for your reference:
Brands that recommend testing in the PM:
- Modern Fertility (Here’s a detailed article explaining why it is ideal in the afternoon)
- Pregmate
- Easy@Home
Brands that recommend testing in the AM:
Brands that recommend testing either in the AM or PM:
- Wondfo (Brand instruction: test between 10 AM and 11 PM, do not use the first urine in the morning)
4. Are there other things to know about the ovulation tests?
- Regardless of which brand you end up choosing, it is important to test at the same time of the day.
- Limit your fluid intake at least 2 hours prior to the tests.
- Once you have started testing, do it for at least 5 days or until the LH surge has been detected.
- Read results at the 5-minute mark.
Some Final Words
We live in a constantly changing world. While we might be focusing on what’s right in front of us (i.e: babymaking), it is important to not lose sight of the bigger environment and be ready to adapt with patience (i.e: the uncertainties accompanying COVID-19.
Ovulation tests can’t guarantee a pregnancy, but they can help you predict what your fertile days are with higher confidence. Also, keep in mind that the general recommendations might not for everyone. It might take several cycles and/or rounds of discussions with your healthcare provider to figure out what works the best for you and your body.
If you find that you’re not able to conceive after 6 months of trying (if you’re 35 years or older), or for more than 1 year (if you’re under 35 years old), don’t hesitate to talk to your healthcare provider.
Like this article? Share it with your loved ones! To get bite-size parenthood wisdom like this, or save infographics for future references, follow us on Instagram (@PMYourParenthood)!
Also, you can support me and my work by contributing a cup of coffee here:


