Our takeaways:
- The labor and delivery process differs by person and perhaps that’s why the pregnancy literature doesn’t seem to be consistent in defining the stages.
- A process flow with general reference points (i.e: cervix dilation, contraction frequency, and duration) for each labor and delivery stage would be helpful for what to expect for both you and your partner.
This morning, we woke up to a happy message that our friend had just given birth to a cute little girl — after 38 hours of labor. While super excited for them, I was somehow caught up by the hours of labor.
I had all these random questions in my head. Was 38 hours long? (I’d imagine it was given all the pain the mom had to endure!) Was it painful from hour 1 all the way to hour 38? If I was in their shoes, how would I know when to leave for the hospital? And when would I be ready to deliver? Also, if my body doesn’t seem to be ready for the hospital, how long do I wait before I should be worried?
Many first-time expectant parents, if not all, would probably have these same questions too. However, the answers, to my surprise, are not quite straightforward. Admittedly, the labor experience is different for every woman (even for the same woman delivering different babies). But if there can be a better-defined process flow to refer to, expectant parents would be more likely to stay calm when labor comes.
Historically, the pregnancy literature doesn’t seem to be consistent in defining labor stages, even among the must-read pregnancy books. For example, some considered “Early labor” as when cervix dilation is between 1 and 3 centimeters (i.e: Expecting Better by Emily Oster). Meanwhile, others considered “Early labor” as when the dilation is between 4 and 6 centimeters (i.e: What to Expect When You Are Expecting by Heidi Murkoff). In this article, we will consolidate the findings using the maximum possible range known across multiple sources to provide a more inclusive reference for labor process flow.
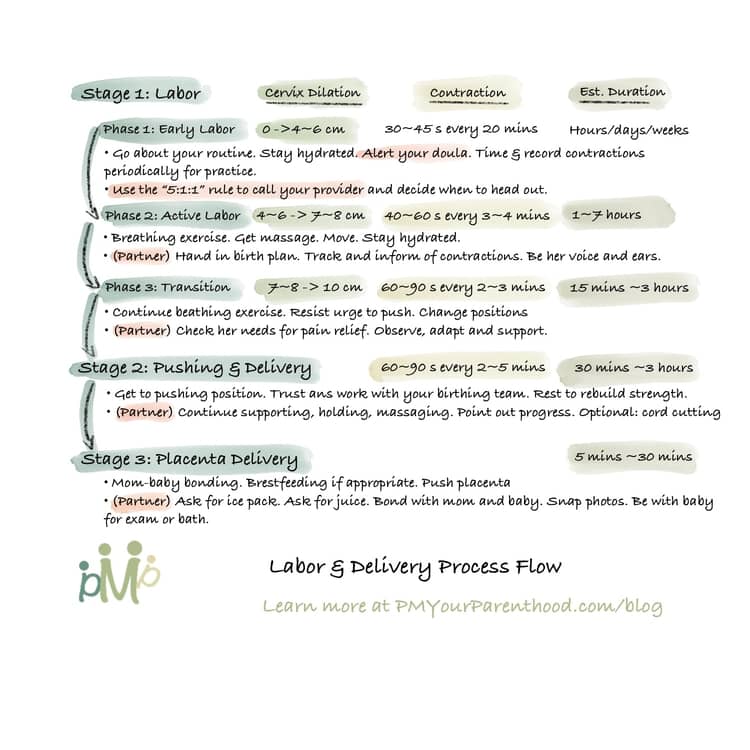
Stage 1: Labor
Phase 1: Early Labor
Cervix dilation: from 0 cm to 4-6 cm
Frequency: can be regular or irregular. Towards the end of this phase, contractions are 30-45 seconds long, 20 minutes apart but will become progressively closer together.
Duration: hours, days, or weeks (often without noticeable contractions)
What can happen: backache, menstrual-like cramps, or none. You may have bloody show (blood-tinged mucus). Your water may break. At this phase, typically you would still be able to talk through contractions.
Actions:
- Go about your usual routine. Stay hydrated (and remember to pee). Alert your doula. Time and record your contractions periodically for practice. Time more frequently when they become 10 minutes apart.
- The “5:1:1” rule – Call your provider when contractions become every 5 minutes, lasting 1 minute long and this has been occurring for at least 1 hour. Also, call your doula to arrange the meetup. Then maybe head to the hospital or birthing center (except for if you are giving birth at home). Note that some providers might prefer a “4:1:2” rule instead (Source). Check with yours to confirm in advance.
Pain relief: Warm shower or heating pad. Tylenol but NO aspirin nor ibuprofen (Advil, Motrin).
Phase 2: Active Labor
Cervix dilation: from 4-6 cm to 7-8 cm
Frequency: can be regular or irregular. Contractions are 40-60 seconds long, 3-4 minutes apart.
Duration: between 1 hour to 7 hours, with average 5-7 hours for first-time delivery and 2-4 hours for experienced delivery.
What can happen: increasing backache, pain/discomfort with contractions. Increasing bloody show. Nausea and/or vomiting. Your water may break if it hasn’t in the previous phase. At this phase, contractions become too strong to talk through (i.e: you’d have to stop mid-sentence to breathe through contractions).
Actions: (You’ll likely be in the hospital/birthing center by now).
- Start breathing exercises. Get a massage from your partner or doula. Stay on the move if you feel like. Ask for pain relief if you need it. Stay hydrated but don’t forget to pee.
- (Your partner) Hand a copy of the birth plan to the nurse. If shift changes makes sure the new nurse is in the loop too. Keep track of the contractions and let mom know when they are about to start and end. If her feet are cold, offer to put on a pair of socks. Be her voice and ears. I highly recommend the partner to read the section “For Dads What You Can Do During Active Labor” in Chapter 14 of “What You Can Expect When You’re Expecting“.
Pain relief: If your water hasn’t break, a warm bath or shower can help ease your pain. Epidural if that’s your choice.
Phase 3: Transition
Cervix dilation: from 7-8 cm to 10 cm
Frequency: contractions are 60-90 seconds long, 2-3 minutes apart.
Duration: 15 minutes to 3 hours
What can happen: this is the most intense part of labor. You may start shaking and shivering. Pressure on your rectum because your baby has usually descended somewhat into your pelvis. Crampy legs. A lot of bloody show. Nausea and/or vomiting. Drowsiness and/or tightening sensation in the throat or chest. Feeling very warm and sweaty or chilled and shaky (or alternate between the two)
Actions:
- Continue breathing exercises. If you feel the urge to push, resist. (Pushing against a cervix that isn’t fully dilated can cause it to swell and delay the delivery.) If you feel too much pressure on your lower back, try changing position(s). You may want all distractions – music or conversation or even that cool cloth or your partner’s loving touch – eliminated in order to concentrate.
- (Your partner) Check in with the mom whether she needs (additional) pain relief and inform the nurse. Observe her body’s reactions and adapt your offer (i.e: cool damp cloth for her forehead or blanket or socks; back massage or staying away from touching her).
Pain relief: adjust and ask for what your body needs (i.e: from no pain relief to needing one; from some epidural to additional)
Stage 2: Pushing & Delivery
Cervix dilation: 10 cm (fully dilated)
Frequency: contractions are still 60-90 seconds long, but more spaced out (2-5 minutes apart) and possibly less painful.
Duration: 10 minutes to 3 hours
What can happen: less intense contractions. Depending on your baby’s position at this point (high or low in your pelvis), you may feel an urge to push (when the baby’s low). You may be instructed to push but you may also want to take it slowly and let your uterus do the work until you feel the urge to push. (Note that epidural can reduce push feeling until your baby’s head has descended quite a bit). As your baby continues to descend and his/her scalp becomes visible, you will feel stronger urges to push and the “ring of fire” (tingling/stretching/burning/stinging sensation) at your vaginal opening. It’s worth noting that pushing doesn’t come naturally for every woman and it’s okay if you don’t feel the urges to push. Turst your birthing team to guide you.
Actions:
- Get into pushing position that you prefer. A semi-sitting or squatting position is often easier with the aid of gravity. It may help to look down past your bump as you push.
- Understand your baby’s movement with your contractions: 2-steps-forward, 1-step-backward, so you don’t get frustrated when your baby’s head recedes.
- At some point, your provider may ask you to push more gently or to stop pushing altogether so your baby’s head has a chance to gradually stretch out your vaginal opening and perineum. A slow, controlled delivery can help keep your perineum from tearing. Pant or blow to counter your urges to push.
- Rest between contractions to rebuild strength.
- (Your partner) Continue supporting her and helping her relax between contractions. Hold her hand or support her back if necessary. If she slips out of position, gently help her back into it. Periodically point out her progress. If you are to cut the cord, know that it can’t be snipped like a piece of string (it’s tougher than you may think).
Stage 3: Delivering the placenta
Duration: 5 minutes to 30 minutes
What can happen: Minutes after giving birth, your uterus begins to contract again. The first few contractions usually separate the placenta from your uterine wall. You may be injected with Pitocin to encourage contractions to speed up placenta delivery and help the uterus go back to size (to stop bleeding). Once the placenta is delivered, your provider will examine the placenta to make sure it’s all there. And if you had an episiotomy or any tears in your perineum, your provider will repair them.
Actions:
- (Now your baby’s out) You can have some skin-to-skin bonding now and/or try some breastfeeding if that’s what you prefer.
- When your caregiver sees signs of separation of the placenta from the uterine wall, s/he may ask you to push to help expel the placenta gently. This is usually one short push that’s not difficult or painful.
- (Your partner) Ask for an ice pack to soothe her perineal area. Ask for some juice for mom. Cuddle and bond with both the newborn and the mom. Capture your baby’s first photos/videos. Accompany the baby for the first exam and bath.
Other notes:
- You might want to think through what type of placenta delivery (active or physiological) you’d prefer beforehand and include your preference in the birth plan.
- You might also want to decide what to do with the placenta.
Like this article? Share it with your loved ones! Or check out similar articles for the delivery stage of your baby.
To get bite-size parenthood wisdom like this, or save infographics for future references, follow us on Instagram (@PMYourParenthood)!
Also you can support me and my work by contributing a cup of coffee here:
